The objective of this article is to explain the relationship between chronic pain and depression, the effect on the family, and to discuss some options for dealing with such pain.
Summary: Pain leads to depression and depression to pain when a chronic pain condition exists. The effects on the family are detrimental to the relationships involved.
It is useful to have an arsenal for dealing with the pain that allows for a minimal use of pain medication as the medication, though it may improve the pain, has side effects that often make the overall situation worse. This article acquaints readers with these issues.
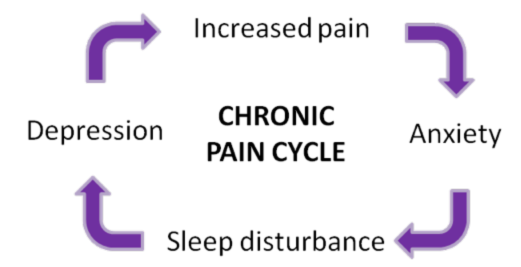
When families have a member who lives in chronic pain, it can affect everyone in the family adversely. The pain can cause the sufferer to be agitated, grumpy, and easily angered. Disruptions of life get over-exaggerated as the person acts out the irritation and the pain as well. Further, the pain can be exhausting. It may disrupt sleep. It may be unrelenting which wears out the individual. This exhaustion creates depression and anxiety which creates more pain as the body tenses. So it becomes a vicious cycle.
People may try to interrupt this cycle with pain medication. Certainly, if medication is required, this article is not about to suggest not taking it. However, the idea is to inform the users of pain medication of what may happen. The pain medication is, for many people, a depressant. In addition, it creates digestive problems resulting in constipation in many people and upset stomachs. The pain may diminish but is replaced by other discomforts which may be just as irritating. And, many pain medications are addicting. This means that higher increments will be needed to address the pain.
People may reach a tolerance point where doctors are unwilling to prescribe more medication or unable to prescribe doses that will be effective. The situation may evolve to looking at other methods of pain control. These suggestions are not meant for people with terminal conditions where comfort is the only goal. The idea is to help people who live in chronic pain to have some quality of life which includes optimizing their relationships with family members. These relationships can be severely affected with chronic pain.
One of my husband's relatives battled pain from arthritis for years. She used a combination of medication, exercise, and rest. She has now added self-hypnosis for pain relief when she has flare-ups. It is working!
My husband's aunt is not alone in trying a form of complementary or alternative medicine to manage chronic pain. There are, according to a recent study, about one third of adults in this country who use some form of alternative or complementary medicine. Chronic pain is the most frequent reason to do so.
Among the divisions of the National Institutes of Health, there is a National Center for Complementary and Alternative Medicine. It defines such medicines as being part of a diverse group of medical and health care systems that aren't considered a part of conventional medicine. Within this group there are five categories:
Alternative medical systems-these include acupuncture and Ayurveda medicine. The latter involves customizing dietary and herbal remedies for the individual and emphasizes the whole person-mind, body, and spirit in treating and preventing disease.
Mind-body interventions-These include meditation and guided imagery and are used to help promote healing by using mental strategies to influence the body.
Manipulation and body adjustment-includes massage and chiropractic.
Biologically based therapies-these include the use of herbs and certain foods that are thought to promote healing.
Energy therapies-these include therapeutic touch and use energy fields to hasten healing.
"Complementary" medicine is different from "alternative" medicine. The former is used ALONG WITH more conventional medicine. The latter is used instead of it. Incorporating either should only be done after careful consultation with your doctor.
In discussing herbs and supplements, an extra caution here. While medicines are regulated by the FDA, the products bought from health food stores are not. Some of those products may be harmless but many are very potent and may interact negatively with traditional medications. Therefore, it is really essential that before taking ANYTHING over-the-counter, that you check with your physician.
Pain is a powerful motivator to seeking alternatives. Sometimes it is the family who is motivated because of the effects on family members and also out fear for the patient and the pain medication addiction factors.
Acceptance of the many complementary and alternative treatments is not uniform in the medical community. Some are accepted and some not, based on scientific data. There are two techniques that are more widely accepted. They are prolotherapy and hypnotherapy.
Hypnosis is an altered state of consciousness, It is brought about by training your mind to focus and then, over time, learning to achieve deeper and deeper state of relaxation. This is a two-fold benefit. it takes the focus off the pain and the relaxation state eases the pain. This technique is best learned with the help of a psychologist or specially trained mental health therapist who has received at least 200 hours of training in this field. Your doctor may be able to help you find the right person.
Hypnosis is commonly used in conjunction with more traditional medicine. As a mind-body therapy, hypnosis appears to influence nerve impulses, hormones, and body chemicals so that affects the manner in which your brain communicates with the rest of your body.
Deep relaxation can be as effective as hypnosis or self-hypnosis. Again, a trained mental health provider should teach this and both of these methods take time to learn effectively.
Pain that affects muscles, ligaments, tendons, bones, and joints can also be a chronic problem. Prolotherapy may be useful here. It involves a series of injections that introduce an inflammatory agent to the affected area. Once injected, the agent causes a temporary low-grade inflammation. It is thought that this inflammation leads to the production of connective tissue which then strengthens loosened tendons or ligaments and results in decreased pain. This method is not meant for use with nerve-related pain or bony pain. It doesn't treat arthritis or muscle pain. Prolotherapy, unlike corticosteroid therapy, actually involves improving the injected tissue by stimulating new tissue growth.
Before, closing, I want to mention the corticosteroid treatments as well. These bring temporary relief and are more used when nerve pain is present such as a pinched nerve in the back. This treatment may last a few months or as much as six to nine months. It must be repeated and some treatments at some times may work better than others. Such treatment is usually better than pain medication for all the reasons discussed earlier. However, amounts of cortisone injections need also to be watched as too much cortisone can kill bones.
There is also biofeedback for pain control and units that electrically stimulate nerves to counter pain. If you or someone you love is in chronic pain and it is adversely affecting them and everyone around them, do consult your physician about alternatives to helping them manage the pain. In this era, with doctors as overwhelmed as they are with patients and paperwork and changing systems, it is the responsibility of the individual to point out problems to the doctor rather than waiting for him or her to be aware of any extended problems that may accompany the medical diagnosis.
